Find a Medicare Part D prescription drug plan

Medicare Part D
Prescription Drug Coverage 2026
Medicare Part D Creditable Coverage Notice
A Medicare Part D creditable coverage notice is a document that informs you whether your current prescription drug plan is as good as or better than a standard Medicare Part D plan. Understanding this notice could be crucial to avoiding future penalties and making informed decisions about your drug coverage.
Key Takeaways
- Creditable coverage might offer prescription drug benefits that may be at least equivalent to Medicare Part D, likely aiding informed decisions about enrollment.
- Employers should provide annual creditable coverage notices by October 15 and report status to CMS, to help ensure compliance with regulatory obligations.
- Non-creditable coverage may result in late enrollment penalties for Medicare, likely making it essential for individuals to maintain creditable coverage.
Understanding Creditable Coverage
Creditable coverage refers to health insurance that might offer prescription drug benefits that may be at least equivalent to those of Medicare Part D. This means that the drug coverage may be expected to provide benefits that may be similar to or better than what Medicare Part D would offer.
Knowing about creditable coverage could help individuals make informed decisions about enrolling in a Medicare Part D plan or continue with their current coverage.
Various types of plans may provide creditable coverage, such as employer or union plans, TRICARE, the Indian Health Service, and the Department of Veterans Affairs. Employers should document whether their drug coverage is creditable compared to Medicare Part D, which will likely involve complex analyses or simplified determination methods allowed by CMS.
For the year 2026, a revised simplified determination method might require group health plan coverage to pay at least 72% of plan participants’ prescription drug costs to be considered creditable. This standard will likely ensure that the coverage provided could meet or exceed the benefits offered by Medicare Part D.
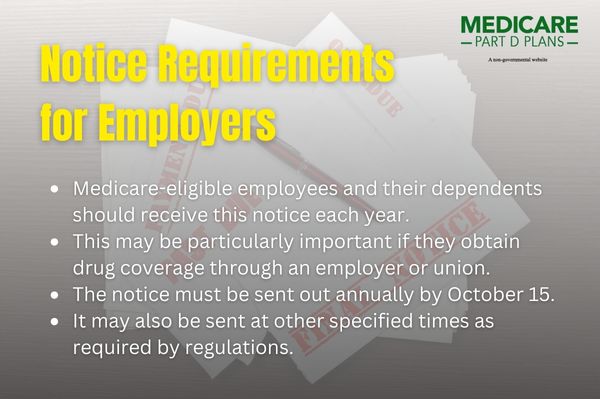
Notice Requirements for Employers
Employers will likely have specific obligations when it comes to providing Medicare Part D creditable coverage notices, for instance:
- Medicare-eligible employees and their dependents should receive this notice each year.
- This may be particularly important if they obtain drug coverage through an employer or union.
- The notice must be sent out annually by October 15.
- It may also be sent at other specified times as required by regulations.
Employers should also provide the Medicare Part D creditable coverage notice to Medicare-eligible individuals when they enroll in the plan. This will likely keep Medicare-eligible individuals informed about their drug coverage’s creditable status, likely aiding in their health coverage decisions.
CMS may also offer model notices that employers could use to effectively communicate the creditable status of their coverage. These notices comply with the Medicare Modernization Act guidelines, which will likely require informing Medicare-eligible individuals about their prescription drug coverage status.
Determining Creditable Coverage Status
Assessing if drug coverage might be creditable will likely involve using accepted actuarial principles and CMS guidelines. One common method has been the actuarial value equivalence test, which may compare the expected paid claims under the employer’s coverage against the standard Part D coverage, where coverage will likely equal the assessment of creditable status.
Employers should show their coverage pays at least 72% of participants’ prescription drug expenses under the revised simplified determination method to provide prescription drug coverage that meets the required standards. This simplified determination could be particularly relevant in 2026 and could potentially ensure that the coverage provided meets the required standards.
Knowing if coverage may be creditable or not will likely be crucial, as it could affect participants’ eligibility for subsidies and may help to avoid late enrollment penalties. Accurately determining and documenting the creditable status of their plans could help employers maintain compliance and effectively support their active employees.
Model Notices from CMS
CMS will likely offer model notices for both creditable and non-creditable drug coverage to help employers and other entities meet notice requirements. These notices may be available for download in both English and Spanish, likely making them accessible to a broader audience.
Entities offering Medicare Part D might customize these templates to clearly communicate the status of their drug coverage to Medicare-eligible individuals, which may include information about generic prescriptions. Using these templates could potentially ensure organizations meet regulatory requirements and provide clear, concise information about their coverage.
Timing and Delivery of Notices
Deliver creditable coverage notices to Medicare-eligible individuals annually before October 15 and at the start of their individual’s initial enrollment period. This timing likely ensures individuals have the necessary information to make informed health coverage decisions.
Acceptable methods for delivering these notices might include mail, email, and in-person delivery. Employers should choose methods that provide reasonable access to the notice and comply with federal law regulatory requirements.
Electronic delivery may be effective as of the effective date if it meets standards ensuring recipients receive and acknowledge the information.
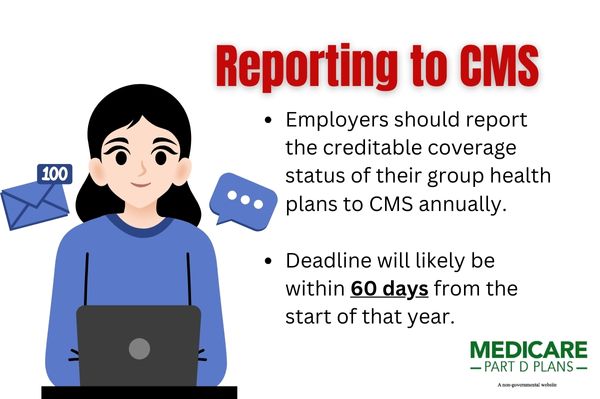
Reporting to CMS
Employers should report the creditable coverage status of their group health plans to CMS annually. This will likely involve submitting the Online Disclosure to CMS Form, detailing the creditable coverage status of their prescription drug plans. The reporting deadline will likely be within 60 days from the start of that year.
Submit the annual report by March 31 each year to ensure CMS has current information on the status of prescription drug coverage provided by employers. Report any changes in the creditable coverage status to CMS within 30 days.
Accurate record-keeping of the delivery of the creditable coverage notice could be crucial for compliance and documentation. Employers must establish effective procedures to compile and report necessary information to CMS, ensuring regulatory compliance.
Potential Impact of the Inflation Reduction Act
The Inflation Reduction Act (IRA) might introduce several changes to Medicare Part D, such as capping cost-sharing for Part D-covered insulin products at about $35 per month. Adult vaccines recommended by the Advisory Committee on Immunization Practices may also be available to Medicare Part D members at no cost.
Additionally, the maximum out-of-pocket costs for prescription drugs under Medicare Part D may be reduced to about $2,000, possibly eliminating the coverage gap, or “donut hole.” This potential change could simplify the coverage stages, likely making it easier for beneficiaries to handle their prescription drug costs.
Possible updates regarding the Medicare prescription drug plan might include:
- Members may be able to spread their out-of-pocket drug costs into monthly payments.
- Part D sponsors should include selected drugs with a maximum fair price on their formularies.
- Plans updated before January 1, 2025, may be re-evaluated for creditable coverage status to ensure compliance with updated Medicare Part D parameters and the drug plan requirements.
See plans in your area instantly!
Advertisement
Retiree Drug Subsidy Program
The Retiree Drug Subsidy (RDS) program will likely offer financial assistance to employers supporting retirees with their prescription drug coverage. This program could help employers maintain drug coverage for Medicare-eligible retirees without major changes to existing benefits.
Employers may also apply for the Retiree Drug Subsidy by applying online through the RDS Center. Employers should apply 90 days before the RDS plan start to ensure timely receipt of the subsidy.
The RDS program could potentially benefit both employers and retirees by managing prescription drug costs and helping to ensure retirees may continue to provide prescription drug coverage without interruption.
Possible Consequences of Non-Creditable Coverage
Creditable drug coverage will likely be crucial to prevent individuals from incurring a late enrollment penalty when they eventually enroll in Medicare Part D. Individuals who do not maintain creditable coverage for 63 days or more after becoming eligible for Medicare may incur a penalty when they enroll in Medicare drug coverage.
These penalties could be significant and will likely have a long-term financial impact, highlighting the importance of maintaining creditable coverage. Maintaining creditable drug coverage could help individuals avoid these penalties and possibly ensure uninterrupted access to necessary medications.
Find a Plan and Enroll Online Yourself!
Advertisement
Summary
Understanding and maintaining creditable coverage under Medicare Part D will likely be essential for avoiding penalties and ensuring that you or your employees could have access to necessary prescription drugs. Employers should provide annual notices, determine the creditable status of their plans, and report this information to CMS.
The possible changes that may be brought about by the Inflation Reduction Act and the potential benefits of programs like the Retiree Drug Subsidy will likely highlight the evolving landscape of Medicare Part D. Staying informed and compliant with these regulations could be crucial for both employers and individuals.
As you navigate these complexities, knowledge and proactive management of your prescription drug coverage could lead to significant benefits and avoid costly penalties. Stay informed, stay compliant, and ensure your coverage meets the necessary standards.
Frequently Asked Questions
What is creditable coverage?
Creditable coverage will likely be a prescription drug plan that may provide benefits at least equal to those of Medicare Part D, possibly ensuring that individuals could have sufficient coverage for their medication needs.
Why might employers need to provide Medicare Part D creditable coverage notice?
Employers may need to provide Medicare Part D creditable coverage notice to inform Medicare-eligible individuals about their drug coverage status, enabling them to make informed decisions and avoid potential penalties. This transparency will likely be essential for compliance and support employees in managing their healthcare choices effectively.
How could employers determine if their coverage is creditable?
Employers may determine if their coverage is creditable by conducting actuarial equivalence testing or applying a simplified determination method to ensure it pays at least 72% of participants’ prescription drug expenses. This assessment will likely be essential for compliance and to ensure proper benefit administration.
What are the penalties for not having creditable coverage?
Failing to maintain creditable coverage for 63 days or more might result in a late enrollment penalty when enrolling in Medicare Part D. It’s crucial to stay informed about your coverage to avoid these financial consequences.
How could the Inflation Reduction Act impact Medicare Part D?
The Inflation Reduction Act may impact Medicare Part D by capping cost-sharing for insulin, providing free vaccines, potentially reducing maximum out-of-pocket costs, and may even eliminate the coverage gap. These changes could potentially ensure more affordable healthcare for beneficiaries.
Begin Choosing your plan
Advertisement
ZRN Health & Financial Services, LLC, a Texas limited liability company.